Introduction
Bleeding disorders, which affect the body’s ability to form clots, can lead to excessive or prolonged bleeding. Conditions such as hemophilia, von Willebrand disease, and platelet function disorders are some of the most common types. Over the years, advancements in medical science have significantly improved the treatment and management of these conditions, offering patients better quality of life and longer life expectancy.
Definition
Most bleeding diseases have a hereditary cause. When the body’s capacity to coagulate blood is compromised, bleeding problems can arise. An inflammatory clot made of platelets and a specific type of blood cell forms on the injured body part. In addition to keeping blood from leaking from the wounded location, this clot keeps pathogens out of the blood. The affected area becomes a breeding ground for various bacterial and viral infections if the body is unable to manufacture the required amount of clots. Massive blood loss can also be a result of serious wounds or infections. Low levels of red blood cells in the body or a lack of vitamin K can also lead to blood diseases.
Understanding Bleeding Disorders
Bleeding disorders occur when the body is unable to clot blood properly, leading to excessive bleeding either externally or internally. The clotting process involves platelets and proteins in the blood, known as clotting factors. When either is missing or not functioning correctly, the blood clotting process is disrupted.
Some of the most common bleeding disorders include:
- Hemophilia: A genetic disorder where the blood lacks clotting factors, specifically factor VIII (hemophilia A) or factor IX (hemophilia B).
- Von Willebrand Disease (VWD): A disorder characterized by a deficiency or defect in the von Willebrand factor, a protein that aids in platelet adhesion.
- Platelet function disorders: These disorders affect the ability of platelets to form clots, even if platelet counts are normal.
While these conditions may vary in severity, they all share one common characteristic: an increased risk of bleeding, which can result in life-threatening complications if not properly managed.
Traditional Treatment Approaches
Historically, treatment for bleeding disorders primarily focused on addressing acute bleeding episodes and preventing complications. Some of the traditional approaches include:
Clotting Factor Replacement Therapy:
For hemophilia, patients receive intravenous infusions of the missing clotting factor, either on-demand (during bleeding episodes) or prophylactically (to prevent bleeds).
Desmopressin (DDAVP):
A synthetic hormone that people with milder types of hemophilia and VWD utilize to induce the release of von Willebrand factor.
Antifibrinolytic Therapy:
Drugs like tranexamic acid are used to prevent blood clots from breaking down, aiding in bleeding control for certain disorders.
Platelet Transfusions:
In cases of severe platelet function disorders, platelet transfusions help restore normal clotting capabilities.
While these treatments have been life-saving, they are often associated with challenges such as frequent infusions, the risk of developing antibodies against clotting factors (inhibitors), and the potential for infections due to blood-based products.
Advancements in Bleeding Disorder Treatments
In recent years, researchers have made significant strides in treating bleeding disorders. These advancements focus on improving patient outcomes, enhancing convenience, and reducing the risk of complications. Here are the key developments you need to know:
1. Gene Therapy
One of the most groundbreaking advancements in bleeding disorders treatment is gene therapy. This innovative approach offers the potential for a one-time treatment that could provide long-term or even permanent relief from symptoms.
- How it works: Gene therapy involves introducing a functional version of the defective gene responsible for the bleeding disorder. In the case of hemophilia, this means delivering a working copy of the gene that codes for the missing clotting factor (either factor VIII or IX) into the patient’s liver cells, which then produce the clotting factor.
- Current progress: Clinical trials for gene therapy in hemophilia have shown promising results, with some patients achieving near-normal clotting factor levels after a single treatment. While gene therapy is not yet widely available, its potential to offer a long-term cure is revolutionary.
2. Extended Half-Life Clotting Factor Products
Traditional clotting factor replacement therapy required frequent infusions, sometimes multiple times a week, which posed a significant burden on patients. However, advancements in biotechnology have led to the development of extended half-life (EHL) clotting factor products.
- Benefits of EHL products: These therapies are designed to last longer in the bloodstream, meaning patients can receive infusions less frequently while maintaining effective clotting factor levels. This improves convenience and adherence to treatment regimens.
- Available options: EHL products are now available for both factor VIII and factor IX replacement, and they have been shown to reduce the frequency of bleeding episodes while offering more flexibility in managing the condition.
3. Non-Factor Therapies
Non-factor therapies represent a new class of treatment for bleeding disorders that do not involve directly replacing the missing clotting factor. One of the most notable advancements in this area is Emicizumab, a monoclonal antibody designed to treat hemophilia A.
- How it works: Emicizumab functions as a bridge between activated factor IX and factor X, imitating factor VIII’s action and allowing blood to clot without the need for factor VIII replenishment. This therapy is administered as a subcutaneous injection, offering a more convenient option compared to traditional intravenous infusions.
- Benefits: Emicizumab has been shown to significantly reduce bleeding episodes in patients with hemophilia A, both in those with and without inhibitors. Its ease of use and effectiveness make it a game-changer for patients seeking an alternative to regular infusions.
4. Inhibitor Management
One of the most significant complications in hemophilia treatment is the development of inhibitors—antibodies that the immune system produces against the clotting factors used in replacement therapy. This makes managing the condition more challenging, as standard treatments become less effective.
- Advances in immune tolerance induction (ITI): ITI is a strategy used to reduce or eliminate inhibitors by exposing the patient to high doses of clotting factors over time. Improvements in ITI protocols and personalized treatment plans have increased the success rate of inhibitor management.
- Bypassing agents: For patients with inhibitors, bypassing agents such as Recombinant Factor VIIa and Activated Prothrombin Complex Concentrates (aPCCs) offer effective alternatives to traditional clotting factors by bypassing the need for factor VIII or IX in the clotting process.
5. Personalized Medicine and Treatment Individualization
Advancements in diagnostic tools and genetic testing have paved the way for personalized medicine in bleeding disorder treatment. By understanding the specific genetic mutations and individual risk factors, healthcare providers can tailor treatments to each patient’s unique needs.
- Pharmacokinetics (PK) profiling: PK profiling involves measuring how a patient’s body processes clotting factor products. This allows for individualized dosing regimens, optimizing the timing and frequency of treatments based on the patient’s specific metabolism.
- Precision therapies: As our understanding of the genetic and molecular basis of bleeding disorders deepens, the development of precision therapies that target specific mutations and pathways is becoming a reality, offering more effective and targeted treatments.
The Future of Bleeding Disorder Treatments
Although researchers have made significant advancements, they are continuing to explore new therapies and refine existing treatments. The ultimate goal is to provide patients with safe, effective, and convenient treatment options that minimize the burden of managing bleeding disorders.
- Next-generation gene therapies: Research is underway to improve the delivery and durability of gene therapies, with the aim of offering even more robust and long-lasting solutions for bleeding disorders.
- Cell-based therapies: Emerging research could revolutionize treatment by genetically modifying patients’ own cells to produce clotting factors for cell-based therapies.
- Comprehensive care models: As treatments advance, there is a growing emphasis on holistic, comprehensive care that addresses the physical, emotional, and social aspects of living with a bleeding disorder.
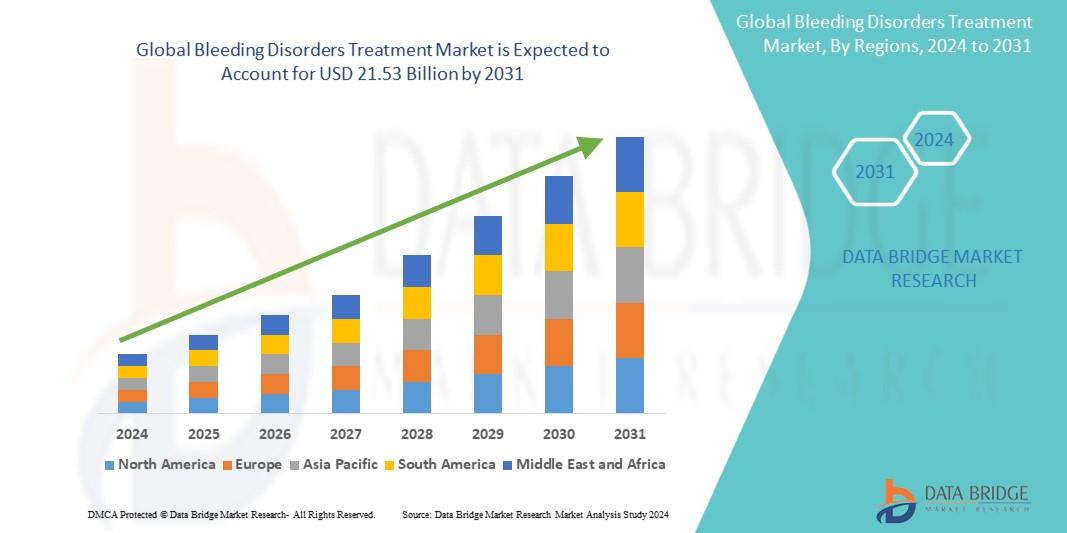
Growth Rate of Bleeding Disorders Treatment Market
The global market for bleeding disorders treatment was valued at USD 10.57 billion in 2023 and is projected to expand to USD 21.53 billion by 2031 at a compound yearly growth rate (CAGR) of 9.3% from 2024 to 2031.
Read More: https://www.databridgemarketresearch.com/reports/global-bleeding-disorders-treatment-market
Conclusion
The landscape of bleeding disorders treatment has transformed dramatically in recent years, offering patients more effective, convenient, and potentially curative options. From gene therapy and extended half-life clotting factors to non-factor therapies and personalized medicine, these advancements represent a new era of care for those living with bleeding disorders. As research continues to push the boundaries of what’s possible, the future holds even more promise for improved outcomes and quality of life for patients.


